Era of Innovation in Structural Heart Intervention
By Dr. Ofir Koren, FACC, FESC, Interventional Cardiologist; Editor-in-Chief of Complex Cases in Structural Heart Intervention (Springer), Specialist in Cardiovascular Innovation, CSMC
In the evolving world of cardiovascular medicine, technology and clinical expertise now work in harmony to address life-threatening heart valve diseases. Structural heart interventions, particularly in the treatment of heart valve pathologies, have seen transformative developments over the past two decades. With the aging population, heart valve diseases like aortic stenosis and valve regurgitation have become increasingly common, particularly affecting patients in their sixties and beyond. This growing challenge has driven innovations in minimally invasive treatments, such as transcatheter techniques that offer a safer and more effective solution for patients who are often too frail for open-heart surgery.
Understanding Heart Valve Diseases
Heart valve diseases are typically divided into two main categories: valve stenosis and valve regurgitation. Aortic stenosis, one of the most common forms of valve disease, occurs when the valve’s opening narrows, making it difficult for blood to flow out of the heart. This places an immense strain on the heart, which must work harder to pump blood. On the other hand, valve regurgitation refers to the failure of a valve to close properly, leading to the backflow of blood and overloading the heart.
For decades, the primary treatment for severe aortic stenosis was surgical valve replacement. While effective, it was not a viable option for many elderly patients due to the high risks associated with major surgery. Traditional surgical aortic valve replacements involved open-heart surgery, which could take four to six hours, followed by months of recovery. Recognizing the unmet need for less invasive alternatives, cardiologists began exploring transcatheter techniques adapted from coronary interventions.
The Advent of TAVR: A Game Changer
Transcatheter Aortic Valve Replacement (TAVR) emerged as a breakthrough solution for patients with severe symptomatic aortic stenosis. Initially developed for patients considered inoperable or at high surgical risk, TAVR has since expanded to include patients across all risk categories. The TAVR procedure involves the insertion of a bioprosthetic valve, which is made partially from animal tissue and specific types of metal, through a catheter into the heart. In contrast to older valves that were entirely metal-based and required lifelong anticoagulation therapy, bioprosthetic valves reduce the need for blood thinners.
The TAVR procedure typically lasts about 90 minutes, and patients can often leave the hospital within days—remarkably shorter than the months of recovery required after traditional surgery. The minimally invasive nature of TAVR has provided new hope for many patients, significantly improving their quality of life and extending their longevity.
One of the most significant advancements in TAVR came with the improvement of pre-procedural imaging. Enhanced CT imaging quality and the use of 3D reconstruction views allowed physicians to better predict potential complications and adjust the procedure accordingly. New delivery profiles were developed, reducing the diameter of the device to minimize vascular injury. Additionally, techniques were devised to navigate calcified and tortuous vessels, addressing anatomical complexities that had previously hindered successful valve implantation.
The era of structural heart interventions is marked by a shift from invasive surgeries to minimally invasive techniques, offering hope and improved outcomes for patients previously considered untreatable.
The Shift Toward Transcatheter Valve Repair
For some patients, neither surgery nor TAVR was a suitable option, prompting the development of transcatheter valve repair techniques. One such approach is Transcatheter Edge-to-Edge Repair (TEER), a procedure used primarily for treating mitral and tricuspid regurgitation. TEER involves the placement of a small clip that adheres the valve leaflets together, preventing them from moving too far apart and causing backflow of blood into the heart.
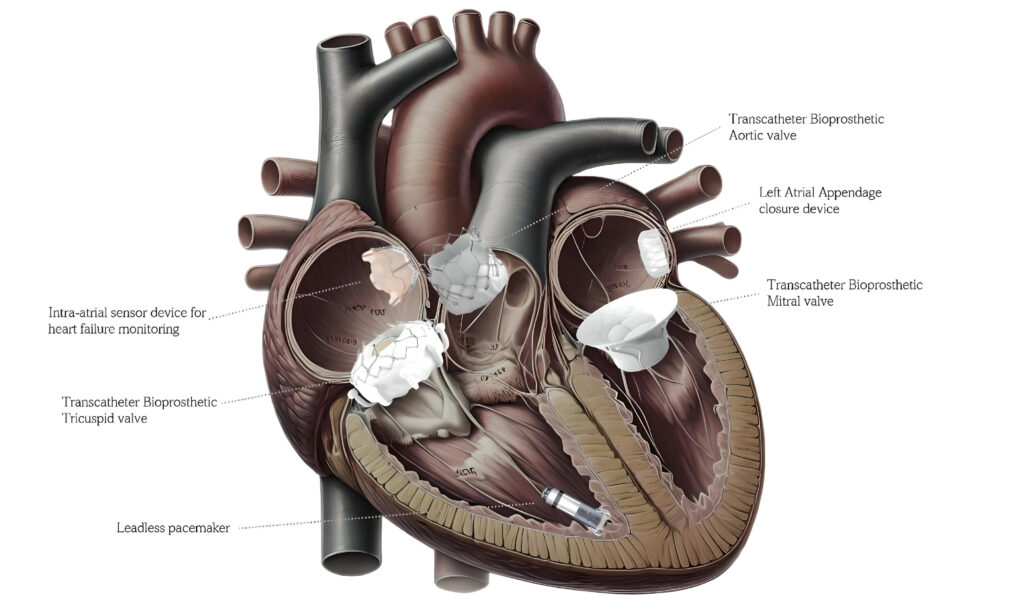
TEER has proven particularly beneficial for patients with functional mitral regurgitation, where the underlying problem lies in the surrounding heart structures rather than the valve itself. The success of TEER and the ongoing advancements in TAVR have inspired further innovations, leading to the development of transcatheter solutions for other valve diseases, such as tricuspid and pulmonary valve replacements.
Looking Ahead: The Future of Structural Heart Interventions
As the field of transcatheter interventions continues to evolve, the focus is shifting toward enhancing valve durability and expanding treatment options for younger patients and those with complex anatomical challenges. The next generation of bioprosthetic valves is expected to last significantly longer, potentially eliminating the need for re-intervention within a patient’s lifetime. Additionally, ongoing research aims to develop new transcatheter devices for treating bicuspid valve disease, severe calcification, and narrow coronary outlets.
While transcatheter interventions have revolutionized the treatment of heart valve diseases, they have also introduced new challenges for the traditional surgical approach. The decrease in the volume of open-heart surgeries has led to a reduction in the number of highly experienced cardiac surgeons, especially those capable of handling the most complex cases. In response, cardiac surgery is evolving as well, with innovations such as robotic-assisted surgery, which minimizes the invasiveness of traditional valve repair and replacement.
Artificial intelligence (AI) has become integral in revolutionizing cardiovascular care, particularly in the field of structural heart interventions. From diagnosis to treatment, AI technologies are now implemented at nearly every stage of patient management. Whether through AI-guided transthoracic echocardiography, coronary lesion detection on CT, or self-controlled robotic transesophageal echocardiography, AI enhances precision and efficiency. AI also aids in monitoring patients at home, predicting complications, and alerting clinicians to potential human errors. The use of AI in cardiology has shortened diagnostic and treatment timelines, while improving the accuracy of data analysis. This technology is regulated under strict guidelines, addressing concerns about its limitations while ensuring that patient care remains under full clinical control. By incorporating AI, the field continues to evolve, offering safer, more reliable, and personalized treatments for a wide range of cardiovascular conditions.
Conclusion
The era of structural heart interventions is marked by a shift from invasive surgeries to minimally invasive techniques, offering hope and improved outcomes for patients previously considered untreatable. Innovations such as Transcatheter Aortic Valve Replacement and transcatheter repair techniques not only expand treatment possibilities but also optimize procedural efficacy by reducing operator learning curves and minimizing potential complications. These advancements improve safety, reduce procedure times and hospital stays, and allow for more accurate patient selection, making these therapies accessible to a wider range of medical centers rather than being confined to a few major institutions. The integration of massive data sets and meticulous image analysis further supports the management of more complex cases that would have previously been rejected. As technology advances, the collaboration between cardiologists, surgeons, and medical engineers will continue to push the boundaries of what is possible in treating heart valve diseases, ensuring that more patients can benefit from life-saving interventions and live longer, healthier lives.

